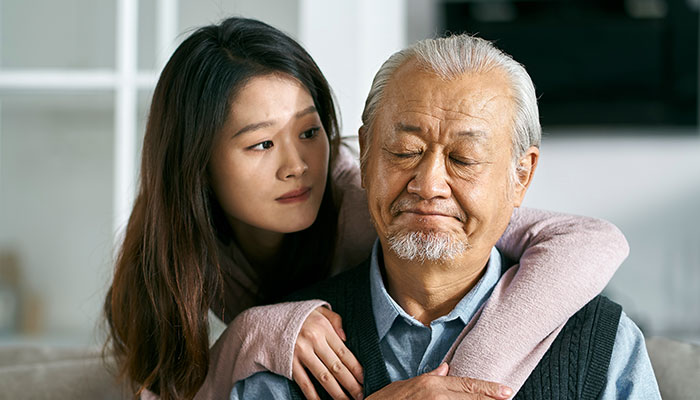
When your parent loses their spouse, both of you are navigating an unfamiliar emotional landscape. Offering a listening ear, supporting new routines, and gently encouraging social connection can help ease the transition. And as you help your parent through their grief, remember to take care of your own feelings too.